More than SAD
The Chicago winter is on its way: the days are darkening earlier, the temperatures will soon plummet and daily tasks may begin to take on an extra level of strenuity. As the end of daylight savings signifies the winter season creeping into Illinois, many begin to throw around the term “seasonal depression.” Doing so addresses the shift in mood many feel in conjunction with the shift in seasons. While the phrase can seem to echo lightly throughout conversations, the reality of seasonal depression carries a heavy weight for many. Seasonal depression is professionally referred to as Seasonal Affective Disorder (SAD), and it may be as misunderstood as it is mislabeled.
As described by the Mayo Clinic, SAD is “a type of depression that’s related to changes in seasons.” While most commonly associated with winter and fall, SAD can also occur during the spring and summer seasons, resulting in the coining of two terms: winter depression and summer depression.
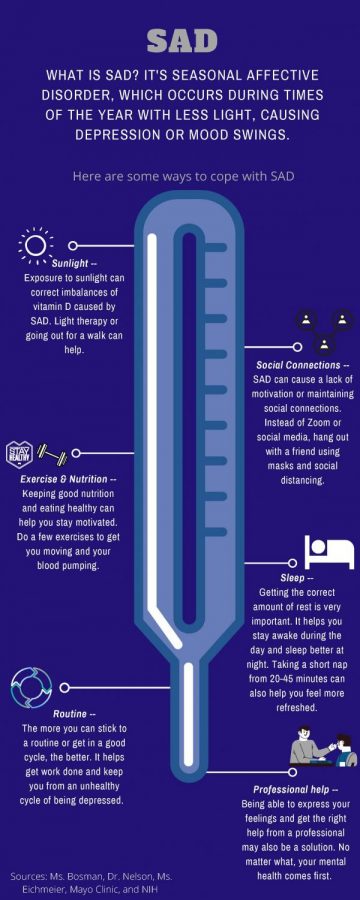
AP Psychology teacher Kara Bosman explained that SAD symptoms are the same as those of major depressive disorder. She added that the only difference between the two mental illnesses is the seasonal onset of SAD. Symptoms include “fatigue, lack of or low arousal, a loss of motivation, or things that used to bring you interest are no longer bringing you interest,” expressed Ms. Bosman.
Brenda Nelson, the LHS prevention and wellness coordinator, added “struggles with sleep” to the list. While the list of symptoms is extensive, a professional diagnosis is necessary to determine if one officially has SAD.
The causes for SAD are largely unknown by scientists, according to The National Institute of Mental Health. Research, however, points mainly towards a reduction in serotonin activity that is caused by the decrease of sunlight in winter. The Hormone Health Network describes serotonin as a regulatory neurotransmitter that “regulates mood, happiness and anxiety.” Sunlight has been found to play a role in the molecular maintenance of serotonin within the body, leaving it capable of impacting well-being. Additionally, many experience a deficiency of vitamin D as a result of less skin-to-sun exposure. This only further impedes the body’s ability to produce and regulate serotonin levels.
Other theorized causes of SAD include the disruption of the circadian rhythm, the natural process that helps maintain a consistent sleep-wake schedule. Although daylight savings is only a one-hour shift, it may be a significant enough impact on the body’s internal cycle to cause SAD. Lastly, as a result of the previous two disruptions, scientists believe bodies will begin to produce excess amounts of melatonin (a sleep regulatory hormone). The shift in melatonin would disrupt sleep quantity and quality, which is known to have an impact on mental health.
Despite the uncertainty of its causes, there are known ways to prevent and combat the effects of SAD. Dr. Nelson recommends “making sure that you’re staying connected with people and making sure that you’re getting the support that you need.”
While staying connected during a pandemic is its own trying and tiring task, it is important nonetheless. Social worker Emily Eichmeier added that “no one should have to experience depression or anxiety at any time of the year. So reach out and don’t feel like you have to try and push it to the side.”
Furthermore, Ms. Bosman encouraged finding new and unique ways to connect with others in order to avoid sitting on yet another Zoom meeting. One recommendation from Ms. Bosman is to find a new and tasty recipe that a friend group can all individually make. This way, it’s possible to share the experience while following all health protocols.
Additionally, Dr. Nelson described the importance of assessing one’s system of connection and support to ensure it is both beneficial and substantial. If not, evaluate options of filling that void. Whether that is sharing feelings with a trusted adult, social worker or close teacher, an essential part of working through SAD is having a supportive network.
It’s similarly important to remember that while “your friends are great…they’re not mental health counselors,” explained Ms. Bosman. If professional help feels necessary, students are encouraged to reach out to a school social worker or trusted guardian.
There are also some individual actions one can take against SAD that are minimal yet beneficial. One potential option recommended by Ms. Bosman is to put effort into receiving vitamin D. Whether that involves phototherapy with the use of UV lights, taking nature walks or simply stepping outside, any effort is a good effort. Another proactive action suggested by Dr. Nelson is to evaluate lifestyle choices to ensure they are beneficial towards well-being. Making health-oriented food, sleep and exercise decisions are encouraged year-round but are even more necessary when entering a season that leaves many prone to mental illness.
While personal health is a top priority, Ms. Eichmeier explained the value in “making yourself available” to support others in this time as well. This includes tasks like checking in with friends and family, offering emotional support and putting effort into conversations. For students, this can mean helping teachers as well. Dr. Nelson explained “it’s just the little things” that students can do in order to help their teachers and their well-being. Dr. Nelson suggested showing appreciation for their effort, speaking up in class and leaving them with a simple “thank you” at the end of the day.
This year in particular presents extra challenges as winter creeps in after months of pandemic isolation, cancellation and anxiety. With the emotions and trials of COVID-19, The Washington Post warns that “pandemic depression is about to collide with seasonal depression” and people should begin to prepare for their own health. In such a high-risk environment, Dr. Nelson stated that those specifically with pre-existing mental health issues should begin taking preventative action against Seasonal Affective Disorder.